LUS is an ultrasound technique that is used to create an image of internal body structures LUNGS. Its aim is often to find a source of a disease or to exclude pathology.
LUS signs, either alone or combined with other point-of-care ultrasound techniques, are helpful in the diagnostic approach to patients with acute respiratory failure, circulatory shock or cardiac arrest.
LUS monitoring can be performed at the bedside and used in mechanically ventilated patients to assess the efficacy of treatments, to monitor the evolution of the respiratory disorder, and to help the weaning process.
LUS can be used for early detection and management of respiratory complications under mechanical ventilation, such as pneumothorax, ventilator- associated pneumonia, atelectasis and pleural effusions.
When LUS can be useful in ER:
- Pleural pathology
- Pericardial pathology
- Shortness of breath
- Cyanosis
- Cough
- Shock
Objectives
- To show the diagnostic capabilities of Lung Ultrasound in Critical Care.
- To illustrate the diagnostic modalities needed.
- To highlight the fields of application.
- To encourage the use of standardized protocols and terminology.

Convex probe

Linear probe

Sector probe
LUS 10 signs:
NORMAL
- Bat sign (pleural line)
- Lung sliding
- A-line (horizontal artifact)
EFFUSION
- Quad sign
- Sinusoid sign
CONSOLIDATION
- Fractal and tissue-like sign
INTERSTITIAL
- B-line (vertical artifact)
- Lung rockets
PNEUMOTORAX
- Abolished lung sliding with stratosphere sign
- Lung point
Two more signs, the lung pulse and dynamic air bronchogram, are used to distinguish atelectasis from pneumonia.
Scoring of findings

NORMAL Lung – A-line
The A-lines are horizontal artifactual repetitions of the pleural line displayed at regular intervals
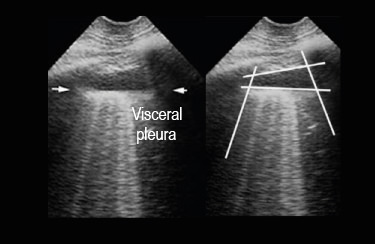
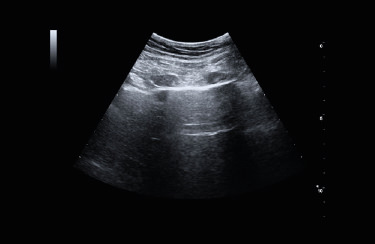
Pleural EFFUSION
Quad sign (2D LUS)
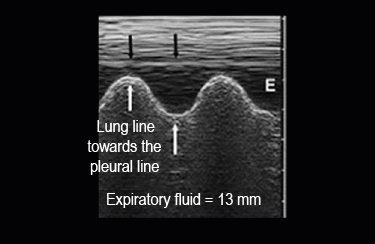
Pleural EFFUSION
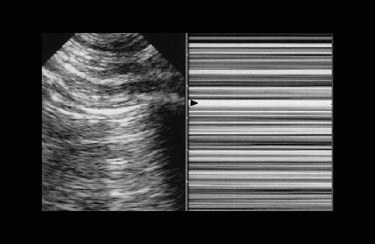
Sinusoid sign (M-mode)

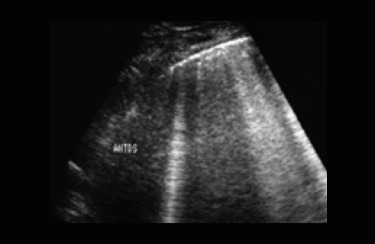
Lung CONSOLIDATION
Massive consolidation of the whole lower lobe without aerated lung tissue and no fractal sign

Lung CONSOLIDATION
Middle lobe consolidation not invading the whole lobe, with fractal border with aerated lung

INTERSTITIAL Syndrome
Pulmonary interstitial edema is designed by diffuse lung rockets. Lung rockets are defined as at least 3 B-lines between two ribs.
PNEUMOTORAX
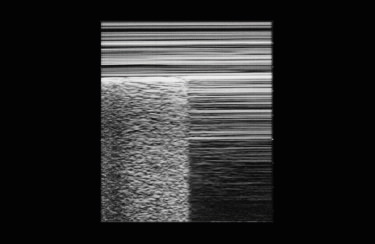
Abolished lung sliding “stratosphere sign”
PNEUMOTORAX
Anterior abolished lung sliding + A-lines

PNEUMOTORAX
Lung point at the area at the junction between dead air pneumothorax) and living air (inflating lung)
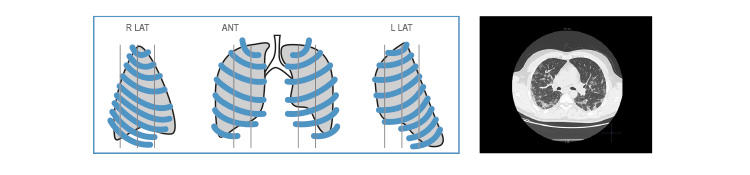
LUNGs approach standardization
Examination technique
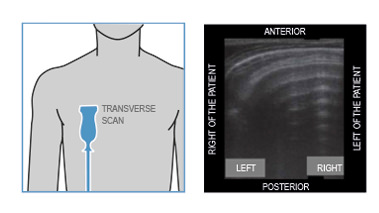
- Patient in a semi-seated and sitting position for optimal access to posterior-basal lung segments.
- Linear probe ( 7.5 -15 MHz) for study of pleural line and subpleural spaces
- Convex probe (3.5 -5 MHz) for B-line evaluation, consolidations and collapses
- Color-Doppler module for assessing vascularization in consolidation
- Appropriate application (abdomen or vascular) with lung preset
- Correct general gain and TGC setting for better B-line representation
- Bilateral lung multiscansions at conventional thoracic lines and between them (parasteral, emiclave, LAA, LAM, LAP) plus posterior scans (scapula angular and paravertebral)
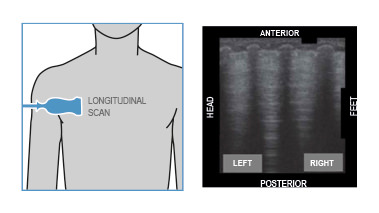
The longitudinal approach has the advantages of locating the pleural line in all circumstances.
CT vs LUS
Lung CT
- Thickened pleura
- Ground glass shadow and effusion
- Pulmonary infiltrating shadow
- Subpleural consolidation
- Translobar consolidation
- Pleural effusion is rare
- More than two lobes affected
- Negative or atypical in lung CT images in the super-early stage, then diffuse scattered or ground glass shadow with the pregress of the disease, further lung consolidation
Lung ultrasound
- Thickened pleural line
- B-lines (multifocal, discrete, or confluent)
- Confluent B-lines
- Small (centomeric) consolidations
- Both non-translobar and translobar consolidation
- Pleural effusion is rare
- Multilobar distribution of abnormalities
- Focal B-lines are the main feature in the early stage and in mild infection; alveolar interstitial syndrome is the main feature in the progressive stage and in critical patients; A-lines can be found in the convalescence; pleural line thickening with uneven B-lines can be seen in patients with pulmonary fibrosis
The ultrasound bedside can read dynamically and constantly the airfluid ratio which the CT scan cannot perform. Lung ultrasound is more sensitive than chest X-ray for the diagnosis of pneumothorax and shows similar high specificity.
- Diagnosis and stage of patient candidates for intubation (forced ventilation)
- Patient follow up (no CT scan )
- Monitoring and adapt fan therapy effectively by avoiding pneumothorax. Rif (Emergency Ultrasound Guidelines 2008) ACEP The medical use of US for diagnostic evaluation of emergency conditions and diagnoses, resuscitation of the acutely ill, Critically ill or injured, guidance of high risk or difficult procedures, monitoring of certain pathologic states and as an adjunct to therapy.
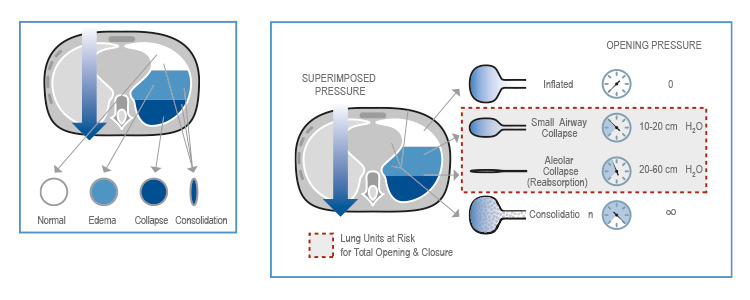
LUS for monitoring mechanical ventilation
Pneumothorax can be a consequence of barotrauma, mainly when lung compliance is reduced. LUS is accu- rate in the diagnosis of pneumothorax (Lichtenstein et al. 2000) and is superior to supine anterior chest x-ray (Blaivas et al. 2005). The presence of real images (consolidation, effusion), of any pleural movement (sliding, lung pulse) or artefacts deriving from the visceral pleura (B-lines) rules out pneumothorax with 100% negative predictive value. If a static A pattern is visualized, a lung point must be searched moving the probe laterally and inferiorly: the lung point corresponds to the site where the collapsed lung goes back in touch with the parietal pleura and rules in pneumothorax with 100% positive predictive value. If no lung point is identified, the positive predictive value of a static A pattern alone ranges from 55 to 98%, depending on the clinical context; for example, if the lung is completely collapsed, no lung point can be visualised.
Our best proposal for LUS

Complete
- High performance in all the applications
- Large probes portfolio, convex, linear and phased-array
- Advanced configurations, including TE probe or Strain package
Fast
- 2 probes connectors Up to 4 with multiconnector
- Touchscreen with intuitive menus
- Long-duration battery and quick boot-up time (15”)
Compact
- Full screen mode
- Swivelling monitor
- Agile trolley easy with 4 swivelling wheels
Connected
- Follow-up & Multi-modality options to retrieve other imaging modalities
- eStreaming for real-time imaging streaming
- eTablet & MyLab™Remote for remote storage and control

Low-frequency probe to scan lung parenchyma and commonly used in emergency for abdominal organs.

High-frequency probe to scan pleural area and superficial structures. Commonly used to scan vessels and support lines’ placement.

Low-frequency phased-array probe to scan the lung and commonly used for heart functionality monitoring.
- Standard care involves handwashing or hand sanitization and use of sterile gloves.
- Droplet precautions include gown, gloves, headcover, facemask and eye shield.
- Airborne precautions add special masks (e.g. N-95 or N-99 respirator masks, or powered air purifying respirator - PAPR systems) and shoe covers.
- Equipment care is critical in the prevention of transmission. Cover probes and machine consoles with disposable plastic and forego the use of ECG stickers.
Echocardiogram machines and probes should be thoroughly cleaned, ideally in the patient’s room and again in the hallway. Smaller, laptop-sized portable machines are more easily cleaned before and after the examination.
Related articles
Ultrasound Systems Cleaning and Disinfection in the event of COVID-19 emergency
This document is provided as an emergency process in response to the outbreak of Coronavirus Disease 2019 (COVID-19) with the aim of preventing virus transmission and simplify and clarify the processes of Cleaning and Disinfecting on site....
COVID-19 emergency
The growing outbreak of COVID-19 has generated unprecedented stress on healthcare systems at global level and the demand of Point-of-Care US in Emergency...
Critical Care examinations made easier during the Covid-19 era
Never stop striving for easy Scanning and easy Quantification in Critical Care in Cardiology, Abdominal, Lung, Vascular, TCD.
Lung Ultrasound in COVID Patients
COVID-19 pneumonia is characterized by alveolar edema with prominent proteinaceous exudates, vascular congestion, patchy inflammatory clusters with fibrinoid material, alveolar epithelial hyperplasia, and fibroblastic proliferation...
Interview to Esaote CEO: “We’ll answer the call of Europe and the USA too.”
First, Esaote came to the aid of China, a country with which the company has strong connections, given that their shares are owned bya group of six Chinese industrial (Wandong, Yuwell, Kangda) and financial companies (Yunfeng, Shanghai Ftz, Tianyi).
Esaote assembles and delivers 103 portable ultrasound scanners in just 3 days
Esaote won a tender launched by Consip on behalf of Civil Protection for the distribution of diagnostic equipment in Italy to face COVID-19 emergency...
The eyes above the masks. Esaote field service engineers
We’ve asked six of them to observe the situation on the front line and share the ways in which their work has changed...
What we can do
We have a duty to develop a complete understanding of the limits within which we can carry out our production activities...
Probes and Agents
The table here included list MyLab™ ultrasound probes and the recommended cleaning, disinfection and sterilization agents and systems...
Covid Webinar - Lung Ultrasound for the Covid-19 era
Covid Webinar - Lung Ultrasound for the Covid-19 era (F. Piscaglia, F. Stefanini, V. Salvatore)...
Interview with Dr. Vito Cianci - Italian version
Interview with Dr. Vito Cianci - Director at Complex Operative Unit, Emergency Department - University Hospital of Padua (Italy) - Italian version (subtitled)
Interview with Dr. Giovanni Battista Fonsi
Interview with Dr. Giovanni Battista Fonsi - Medical Director at Emergency Surgery Department - DEA, Policlinico Umberto I, Rome (Italy) - Italian version (subtitled)
Interview to Lorenzo Leogrande
A cultural and technological revolution is affecting almost all areas of healthcare. Has COVID-19 become a kind of accelerator for this transformation? What does an experience like this one teach us, in particular with regard to a correct use of technology?
How to protect the ultrasound
In this video we are going to show you how to cover the ultrasound system in order to perfom in a secure and safe way the Lung Ultrasound examination to the patients affected by Covid-19.
Interview with Dr. Carla Serra
Interview with Dr. Carla Serra - Head of the Departmental Interventional Ultrasound Programme at Policlinico Sant’Orsola Malpighi in Bologna (Italy) - Italian version
Esaote Ultrasound Probes Cleaning and Disinfection in the event of COVID-19 emergency
Ultrasound is among the imaging techniques that involves the greatest interaction between physician and patient. This greatly benefits diagnostics, allowing continuous interaction and a fruitful exchange of information between doctor and patient.
COVID-19 and the Heart
Cardiac involvement is a prominent feature in COVID-19 and is associated with a worse prognosis...
Interview with Prof. Fabio Piscaglia
Interview with Prof. Fabio PIscaglia - Director of Internal Medicine at Bologna’s Sant’Orsola-Malpighi General Hospital
Poster on Covid-19 Pneumonia - Lung Ultrasound
Covid-19 Pneumonia - Lung Ultrasound (LUS) assessment of severity of involvement (F. Piscaglia, F. Stefanini). LUS helps estimate the severity of peripheral lung involvement in COVID-19, contributing to quicker and more solid patient management.
Lung Ultrasound Protocol
Esaote technologies are always at your side to support healthcare professionals and make critical examinations easier, allowing diagnosis and follow-up of lung involvement in COVID patients.
Discover the "Lung Ultrasound Protocol", our focused solution in the fight against the Covid-19.
Interview with Pr. Libertario Demi
Let’s talk about the Esaote Solution for the Lung Ultrasound examination. We will present the new MyLab™ Lung Ultrasound Protocol and the technology behind it...






















