COVID-19 pneumonia is characterized by alveolar edema with prominent proteinaceous exudates, vascular congestion, patchy inflammatory clusters with fibrinoid material, alveolar epithelial hyperplasia, and fibroblastic proliferation. These histopathologic changes provide a particular pattern of findings on lung ultrasound (LUS) that can help to differentiate COVID pneumonia from other causes of acute dyspnea.
LUS allows a bedside examination of patients, even those who are critically ill, without needing to transfer them. Thus, it could represent a valuable approach for the diagnosis and follow-up of lung involvement in COVID patients, minimizing the risk of further infection in healthcare personnel.
In particular, LUS can be used for:
- triage of symptomatic patients at home or in the emergency room
- prognostic stratification and monitoring of patients with COVID pneumonia
- monitoring of ICU patients with ventilation
- monitoring of therapeutic interventions
Since this global emergency needs a unified approach, Italian experts in LUS involved in the management of COVID-19 patients in different areas of Italy (Lucca, Trento, Rome, Pavia, Brescia, Voghera, Lodi) proposed a standardized acquisition protocol and scoring algorithm.
Acquisition Protocol (1/2):
- portable US, wireless probe, tablet
- all devices wrapped in single use plastic covers to reduce the risk of contamination and to facilitate the sterilization procedures
- 2 operators – one operator performing the examination, the second with tablet at safe distance from the patient
- convex or linear probes, according to the patient’s body size
- single focal point modality (no multi-focusing), setting the focal point on the pleura line
- low mechanical index (MI) (start from 0.7 and reduce it further if possible), high MIs, if employed for a long observation time, may result in damaging the lung
- avoid saturation phenomena as much as possible by controlling the gain
- avoid the use of cosmetic filters and specific imaging modalities such as Harmonic Imaging, Contrast, Doppler, Compounding
- achieve the highest frame rate possible
- save the data in DICOM format
Acquisition Protocol (2/2):
14 standard areas are proposed to be scanned in each patient, using landmarks on chest anatomic lines (see the scheme). In patients able to maintain a sitting position:
- Right basal on paravertebral line above the curtain sign
- Right middle on paravertebral line at the inferior angle of shoulder blade
- Right upper on paravertebral line at spine of shoulder blade
- Left basal on paravertebral line above the curtain sign
- Left middle on paravertebral line at the inferior angle of shoulder blade
- Left upper on paravertebral line at spine of shoulder blade
- Right basal on mid-axillary line below the internipple line
- Right upper on mid-axillary line above the internipple line
- Left basal on mid-axillary line below the internipple line
- Left upper on mid-axillary line above the internipple line
- Right basal on mid-clavicular line below the internipple line
- Right upper on mid-clavicular line above the internipple line
- Left basal on mid-clavicular line below the internipple line
- Left upper on mid-clavicular line above the internipple line
In patients on invasive ventilation and in patients that are not able to maintain a sitting position, the posterior areas might be difficult to be evaluated. In these cases, the operator should try to have a partial view of the posterior basal areas and start echographic assessment from landmark number 7.
* Protocol, schemes, and figures are reproduced by kind permission of the corresponding author of Wiley Global Permission OfficeProposed Areas for Lung Scanning

Scoring of findings

Score 0
The pleura line is continuous, regular and horizontal artifacts (A-lines) are present.

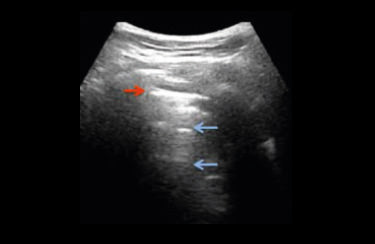
Score 1
The pleura line is indented and below the indent are visible vertical areas of white, which reflect local alterations in the acoustical properties of the lung caused by a replacement of air by water, blood, or fibrous tissue.

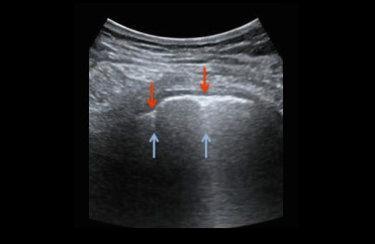
Score 2
The pleura line is broken; below the breaking point are small to large consolidated areas (darker areas) associated with areas of white. The darkening of the consolidated areas indicates the loss of aeration; white areas indicate the presence of air embedded in tissue like material.


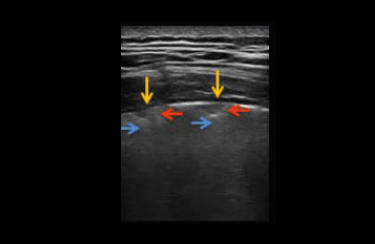
Score 3
The scanned area shows dense and largely extended white lung with or without consolidations.
At the end, the physician indicates the highest score obtained for each area.
International database for data storage, image analyses, artificial intelligence studies
The authors of the article encourage the scientific community to embrace the development of a protected, internationally available database that allows the upload of images and videos of COVID-19 patients (X-ray, ultrasound, and CT scan).
This will speed the development of dedicated pattern recognition algorithms able to recognize COVID-19 related pathological findings, allow for the comparison between different centers, and foster the development of telemedicine programs (including remote evaluation of images, clinical advice, and case discussions) and telematic teaching programs.
https://covid19.disi.unitn.it/iclusdb
Our best proposal to fight against Covid-19

Complete
- High performance in all the applications
- Large probes portfolio, convex, linear and phased-array
- Advanced configurations, including TE probe or Strain package
Fast
- 2 probes connectors Up to 4 with multiconnector
- Touchscreen with intuitive menus
- Long-duration battery and quick boot-up time (15”)
Compact
- Full screen mode
- Swivelling monitor
- Agile trolley easy with 4 swivelling wheels
Connected
- Follow-up & Multi-modality options to retrieve other imaging modalities
- eStreaming for real-time imaging streaming
- eTablet & MyLab™Remote for remote storage and control

Low-frequency probe to scan lung parenchyma and commonly used in emergency for abdominal organs.

High-frequency probe to scan pleural area and superficial structures. Commonly used to scan vessels and support lines’ placement.

Low-frequency phased-array probe to scan the lung and commonly used for heart functionality monitoring.
Bibliography
- Proposal for international standardization of the use of lung ultrasound for COVID-19 patients; a simple, quantitative, reproducible method.
Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T,
Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F,
Demi L J Ultrasound Med. 2020 Mar 30. doi: 10.1002/jum.15285.
Related articles
COVID-19 emergency
The growing outbreak of COVID-19 has generated unprecedented stress on healthcare systems at global level and the demand of Point-of-Care US in Emergency, ICU and CCU departments dramatically increased due to unexpected number of critical patients to be monitored. Interstitial lung disease is a life-threatening complications of COVID infection...
Critical Care examinations made easier during the Covid-19 era
Never stop striving for easy Scanning and easy Quantification in Critical Care in Cardiology, Abdominal, Lung, Vascular, TCD.
Interview to Esaote CEO: “We’ll answer the call of Europe and the USA too.”
First, Esaote came to the aid of China, a country with which the company has strong connections, given that their shares are owned bya group of six Chinese industrial (Wandong, Yuwell, Kangda) and financial companies (Yunfeng, Shanghai Ftz, Tianyi).
Esaote assembles and delivers 103 portable ultrasound scanners in just 3 days
Esaote won a tender launched by Consip on behalf of Civil Protection for the distribution of diagnostic equipment in Italy to face COVID-19 emergency.
The eyes above the masks. Esaote field service engineers
We’ve asked six of them to observe the situation on the front line and share the ways in which their work has changed.
What we can do
We have a duty to develop a complete understanding of the limits within which we can carry out our production activities.
Probes and Agents
The table here included list MyLab ultrasound probes and the recommended cleaning, disinfection and sterilization agents and systems
Covid Webinar - Lung Ultrasound for the Covid-19 era
Covid Webinar - Lung Ultrasound for the Covid-19 era (F. Piscaglia, F. Stefanini, V. Salvatore)
Interview with Dr. Vito Cianci
The emergency room is the front office of the hospital. The doctors who work there are used to making quick decisions: what has changed with the Covid-19 emergency? What are the potentials and limitations of lung ultrasound?
Interview with Dr. Giovanni Battista Fonsi
In the daily management of the COVID-19 emergency, was it necessary for health professionals to review their way of doing ultrasound? How important is it to be able to carry out assessments on multiple districts, if necessary, through ultrasound?


